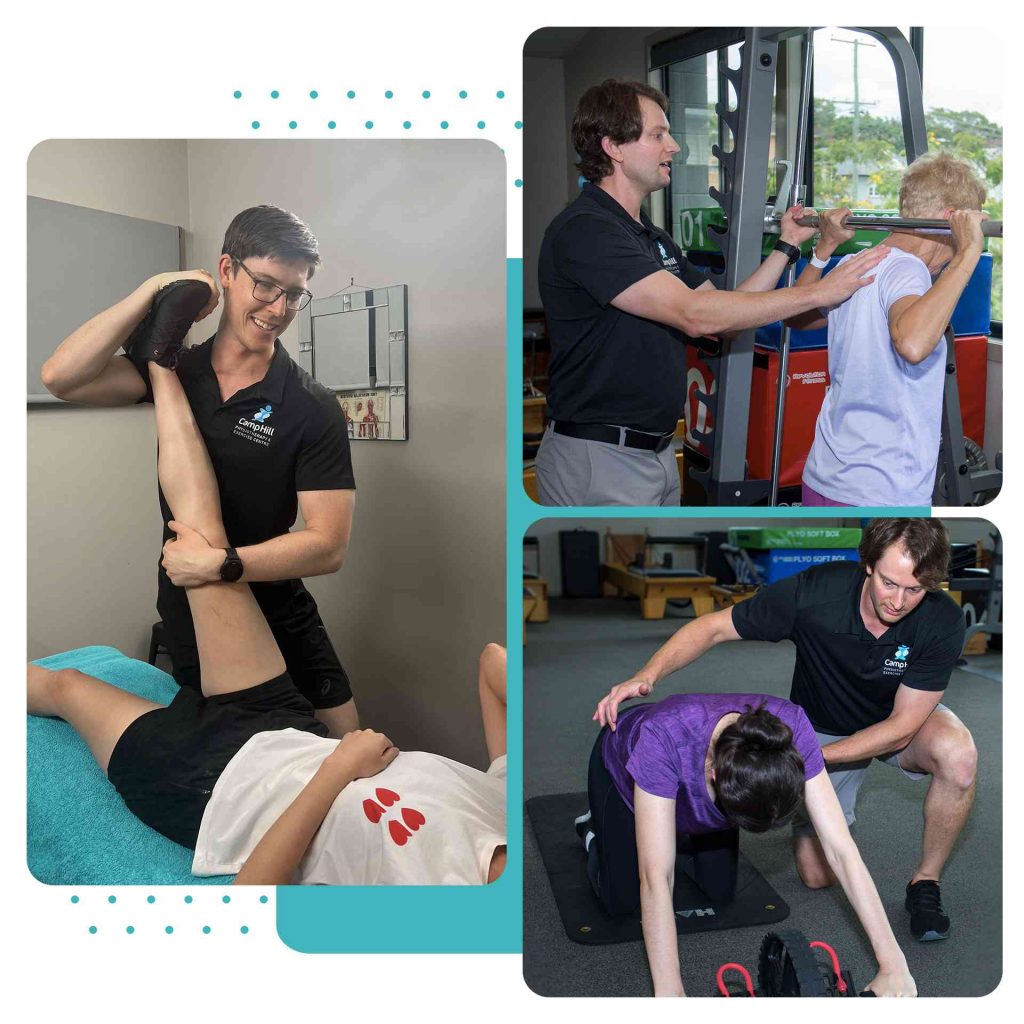
Empowering You to Move & Feel Your Best
Our family-owned clinic is dedicated to providing you with personalised care and the support you need to achieve your rehabilitation and wellness goals.
Oliver Bellwood
Exceptionally professional and courteous staff, every visit I've had has been efficient and effective, I highly recommend!
Matt Rutter
Nick is an amazing Physio who is able to solve injury problems and get me back out in the park asap
Mabel Wai
Lovely, friendly clinic. Such dedicated and passionate staff.
Kate Lupton
I have been treated by both Peter and Nick at the clinic and both experiences have been amazing. They have both made me feel very comfortable and have explained my injuries and treatment plans to me, making sure I understand and feel confident to take on rehab. They are both very knowledgeable and have a passion for physio, I felt they really cared about my recovery. I feel confident getting back onto the court after rehabbing my injuries with both the boys. They are my go to for any netball injury and I always leave feeling more confident and at ease to get back into sport.
Jodie McLean
I love love love Camp Hill Physio, and all of the staff. Sharon Soden is the most incredible Pilates Instructor. I think she is the best instructor I have ever worked with. I cannot recommend her enough.
sandra gartside
Nick is very knowledgeable and provides excellent service.
Kristie Whitcombe
Had an initial consultation with Nick today to alleviate the pain of tennis elbow from 30 years of hairdressing. He was amazing! I left more comfortable and more knowledgeable about how to look after myself between visits.
Highly recommended. Thanks Nick!
Fiona Lane
Last minute appointment and wasn't disappointed. Met all expectations, follow up exercises were explained thoroughly and supported by the physioapp. Thank you